COVID-19 Resources
Opelousas General Health System continues to monitor the Coronavirus (COVID-19) outbreak closely to ensure our community's preparedness. Please know we are committed to caring for our patients and ensuring we respond to the healthcare needs of our community.
Click Here for information on the COVID-19 Vaccine
UPDATED VISITOR INFORMATION
Updated 9/7/2022
Opelousas General Health System has updated our Visitor Policy. We ask that you not visit if you are experiencing any COVID-19 symptoms. Although we have identified areas of visitation, these decisions are subject to change based on the needs of the patient as well as department activity. Our goal is to support our patients as well as our patients’ families. We appreciate your understanding.
- Adult Medical/Surgical Units - one visitor is allowed to stay overnight with the patient.
- Labor and Delivery/Obstetrical/Nursery Units - Should the patient desire, two visitors at a time are permitted during the labor and delivery process. A third visitor can be allowed at the request of the patient. One visitor is allowed to stay overnight with the patient.
- Emergency Department - One adult visitor will be allowed in the ED room with the patient. For pediatric patients, two caregivers can accompany the patient.
- Intensive Care Unit - Once the patient has been assessed by the nursing staff and stabilized, family visitation will be allowed.
Click here to read the full updated policy.
COVID-19 SYMPTOMS
- Fever
- Cough
- Shortness of breath
- Chills
- Muscle Pain
- New loss of taste or smell
- Sore throat
WHAT TO DO IF YOU'RE SICK
If you develop fever, cough and/or shortness of breath, and have been in close contact with a person known to have COVID-19, Call your primary care doctor. If you don’t have one, please call Opelousas General Health System at (337) 948-3011.
UPDATED MASK INFORMATION
For the safety of our patients and staff, we recommend patients and visitors that are not vaccinated to wear a mask. Updated 7/14/2022.
COVID testing prior to procedures/outpatient testing:
Beginning Monday, April 5, 2021, patients will no longer required to be swabbed for COVID prior to surgery, sleep studies, PFT testing, speech testing or cardiac cath lab procedures.
Patients will continue to be screened by being asked the COVID questionnaire and
following the appropriate protocol should patient have symptoms or have
been exposed to
someone with COVID.
COVID-19 CONVALESCENT PLASMA DONATIONS
Plasma from recovered COVID-19 patients can be used to help treat critically ill patients. If you have had a documented diagnosis of COVID-19 by a molecular PCR test and are now recovered and asymptomatic, please call 337 943-7180 to find out if you qualify as a donor. To learn more, visit http://www.lifeshare.org/faqs
SUPPORT OGHS
The American Hospital Association has launched a "Protect the Heroes" campaign which allows the general public to make direct impact donations to America's hospitals/health systems. Every dollar raised from Protect the Heroes goes directly to the donor’s choice of local hospital to purchase personal protective equipment (PPE) and other support for their local healthcare workers to fight COVID-19.
Visit www.protecttheheroes.org to be connected to a local hospital and contribute to hospital emergency relief funds. Each hospital will determine where funds should be applied.
RESOURCES
Children's Resources:
- Explaining Death to Children when Someone Dies due to COVID-19
- Explaining Germs COVID to Children
- Helping Children Say Goodbye From Afar
- Supporting Children and Teens When Someone is Dying
CDC Resources:
Community Resources:
THANK YOU TO OUR COMMUNITY
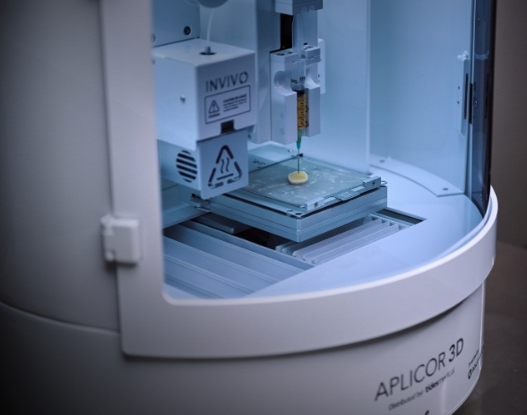
The Wound Treatment Center at Opelousas General Health System Is Saving Lives using Hyperbaric Oxygen Treatment!
The Wound Treatment Center at Opelousas General Health System is the only facility in the state of Louisiana, and one of only a handful in the country that uses Hyperbaric Oxygen Treatment (HBOT) for patients diagnosed with COVID-19 to prevent mechanical ventilation.
Dr. Kerry Thibodeaux, FACS, CWSP, FAPWCA, initiated HBOT early on as a successful means of treatment. “It differs from ventilator treatment because it doubles the atmospheric pressure, thus doubling the amount of oxygen that enters the lungs and the blood stream. Oxygen binds to red blood cells, and is delivered throughout the body, but when it is received in the body under pressure, it also dissolves in the plasma, which greatly increases the oxygen level in the blood stream. This allows cells to work normally, crucially boosting the anti-inflammatory response which helps the patients lungs recover greatly benefiting the healing process,” he explained.
The video link below features Dr. Thibodeaux in a television interview with KALB in Alexandria and further explains the treatment procedure of HBOT.
Dr. Thibodeaux continues to educate medical executives throughout the country and the world about HBOT for COVID-19 patients. Recently, he served as faculty in a webinar, entitled “Evidence Review for HBO2 Treatment of Covid-19” along with Marcus Speyrer, RN, CWS, DAPWCA, Chief Operating Officer of The Wound Treatment Center for the Undersea & Hyperbaric Medical Society, which is the United States governing body for Hyperbarics. Dr. Thibodeaux shared data from previously treated patients, while Speyrer shared best practices for infection control and transporting patients. Faculty from Australia, Sweden, Italy and Australia were also in attendance.
This video highlights the work that Dr. Kerry Thibodeaux is doing regarding treatment for COVID-19 patients. https://youtu.be/jG2LBW4mpNk
Infection Prevention Guidance on Mask Use and Re-Use
To Remove Facemask with intent to reuse:
- Perform hand hygiene
-
Remove mask
- Remove an ear loop style mask by holding the ear loops. The front is contaminated, so remove slowly and carefully.
- Remove a tie style mask by untying lower ties FIRST. Untie upper ties last. The front is contaminated, so remove slowly and carefully. Ensure ties do not fall into clean interior side of mask.
- After removing facemask, visually inspect for contamination, distortion in shape/form. If soiled, torn, or saturated the mask should be discarded.
- If the facemask is NOT visibly soiled, torn, or saturated, carefully store on a paper towel exterior side of mask down.
- Perform hand hygiene.
To Re-Don Mask
- Perform hand hygiene
-
Grasp mask
- Pinch an ear loop style mask at the ear loops or
- Grasp a tie style mask by upper ties on surgical mask
-
Place over face
- For ear loop style mask: Secure ear loops behind the ears. Secure mask.
- For tie style mask: Secure upper ties first, behind head.
- End by securing lower ties behind head.
- Perform hand hygiene.

[1].jpg)

.jpg)
.jpg)